Abstract
Objectives: To clarify the biological characteristics of bone marrow mesenchymal stromal cells (MSCs) in Ph+ acute lymphoblastic leukemia (Ph+ ALL) patients in different disease states, and compare protective effects of MSCs in different disease states on leukemia cells and explore the possible mechanisms.
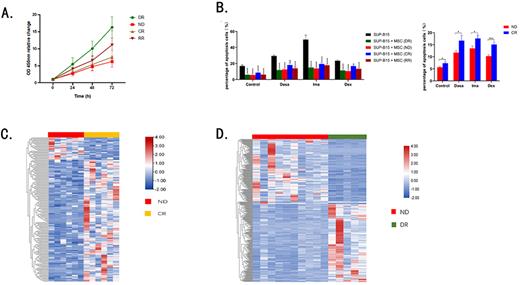
Methods: Bone marrow specimens from Ph+ ALL patients in various disease status (newly diagnosis, complete remission, relapse/ refractory) and healthy donors were collected. Bone marrow mononuclear cells (BMNCs) were isolated and cultured for primary MSCs. (1) CCK-8 method was used to compare proliferation ability of MSCs in vitro. (2) IC50 concentrations of dasatinib (Dasa), imatinib (Ima) and dexamethasone (Dex) in SUP-B15 were determined. SUP-B15 were co-cultured with HS-5 (a human stromal cell line) and MSCs respectively, then the apoptosis ratio of SUP-B15 cells after drug treatment was detected. (3) Transcriptome sequence (RNA-seq) of MSCs was performed, and differentially-expressed genes (DEGs) and signal pathway enrichment analysis among MSCs and BMNCs groups were performed. (5) qRT-PCR was used to detect the expression levels of candidate genes in MSCs.
Results: (1) The proliferation ability of DR-MSCs in vitro was stronger than ALL-MSCs (P<0.01, Figure 1A). Proliferation ability of MSCs from refractory and relapsed group (RR-MSCs) were stronger than that from complete remission group (CR-MSCs) and newly diagnosed group (ND-MSCs)(P<0.05, P<0.05, Figure 1A). There was no significant difference between newly diagnosed-complete remission (ND-CR) paired MSCs (P>0.05). (2) The ratios of apoptotic SUP-B15 cells were significant decreased when co-cultured with HS-5 with and without the presence of Dasa, Ima, and Dex (P<0.05, P<0.0001, P<0.001, P<0.01, Figure 1B). (3) Ratios of apoptotic SUP-B15 cells were significantly reduced when co-cultured with different MSCs under the treatment of blank control, Dasa, Ima, and Dex. The abilities to prevent SUP-B15 cell apoptosis of DR-MSCs and ND-MSCs was stronger than that of CR-MSCs (P<0.001, P<0.05, P<0.01, P<0.0001, P<0.05, P<0.05, P<0.05, P<0.001) (Figure 1B). (4) The RNA-seq results showed that the gene expression thermogram among DR-MSCs, ND-MCSs and CR-MCSs were quite different (Figure 1C-D). Expression of BMP4 in ND-MSCs was significantly up-regulated (FC=3.311, P. adj=0.024) comparing with DR-MSCs. RR-MSCs expressed higher level of BMP4 than CR-MSCs (P<0.05). The expression level of BMP6 in CR-MSCs was lower than that in ND-MSCs (P<0.05). DEGs were mainly enriched in BMP/SMADs signaling pathway by GO enrichment analysis (P. adj<0.0001). (5) Comparing with DR-MSCs, DEGs in ND-MSCs were enriched in cytokine receptors and immune gene-related pathways by Reactome enrichment analysis (P. adj=0.023). (6) TIDE scores of CR-MSCs and RR-MSCs were higher than those of ND-MSCs (P=0.045 and P =0.06, respectively).
Conclusion: Compared with DR-MSCs, Ph+ ALL-MSCs had a weaker proliferative capacity in vitro. MSCs derived from different disease status have protective effects on the apoptosis of SUP-B15 induced by drugs, the effects of DR-MSCs and ND-MSCs were stronger than that of CR-MSCs. The protective effect may be achieved through the activity of BMP/SMADs signaling pathway.
Figure Legend: A. In Vitro proliferation of MSCs;B.The effect of MSCs cells on apoptosis of SUP-B15;C.Differential gene expression thermogram of DR-MSCs and ND-MCSs;D.Differential gene expression thermogram of ND-CR compared samples.
Disclosures
Wang:AstraZeneca: Consultancy; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal